What Happens To Your Labia During Menopause: A Gentle Guide To Changes Below
Menopause marks a significant shift in a woman's life, a natural progression that brings about many physical and emotional adjustments. While hot flashes and mood shifts often get much of the attention, there are also less discussed, yet equally important, changes that occur within your intimate anatomy. Understanding what happens to your labia during menopause can help you feel more prepared and in control during this time of life. It's truly a journey of discovery for your body, so to speak.
For many, the idea of changes to their private parts can feel a bit unsettling, or perhaps even a little embarrassing to talk about. Yet, knowing what to expect is a powerful tool for self-care and maintaining your comfort. Just as "My text" highlights the importance of seeking knowledge and understanding about life's big questions, we aim to provide clear, compassionate information on a topic many wonder about, but might not feel comfortable asking directly. It’s about shedding light on a part of your body that, frankly, experiences a lot of quiet transformations.
This article is here to offer a warm, straightforward conversation about the intimate changes you might notice as your body moves through menopause. We'll explore the specific ways your labia can change, why these shifts occur, and what you can do to manage any discomfort. It’s all about empowering you with facts and helpful approaches, because, you know, feeling good in your own skin, no matter the stage of life, is really what matters.
Table of Contents
- What Exactly Are the Labia?
- The Menopause Transition: A Quick Look
- What Happens to Your Labia During Menopause?
- Why Do These Changes Occur?
- Managing Labial Changes: Practical Tips and Support
- Dispelling Common Concerns and Embracing Change
- Frequently Asked Questions
- Conclusion
What Exactly Are the Labia?
Before we discuss what happens to your labia during menopause, it's helpful to understand what these parts are and their role. The labia are the folds of skin that protect the clitoris, urethra, and vaginal opening. They are a significant part of the vulva, which is the external female genitalia. You know, the parts you see on the outside.
Labia Majora: The Outer Folds
These are the larger, outer folds of skin that typically have pubic hair. They are somewhat fleshy and protective, shielding the more sensitive inner parts. Think of them as the first line of defense, so to speak, for the delicate structures within. They are, quite simply, a very important part of your anatomy.
Labia Minora: The Inner Folds
Located just inside the labia majora, these are the smaller, hairless folds of skin. They vary greatly in size, shape, and color from person to person. These inner folds surround the vaginal and urethral openings, and are quite sensitive, playing a role in sexual sensation. They are, in a way, like delicate curtains for your intimate areas.
Why They Matter
Beyond their role in sexual pleasure, the labia provide a physical barrier against irritants and infections. They help keep the delicate internal tissues moist and protected. So, their health and comfort are, naturally, quite important for overall well-being. They really do a lot of quiet work, you know.
The Menopause Transition: A Quick Look
Menopause isn't just a single event; it's a gradual process that typically spans several years. It begins with perimenopause, where your body starts to prepare for the end of its reproductive years, and culminates in menopause, defined as 12 consecutive months without a menstrual period. This whole period, you see, is a big shift for your body.
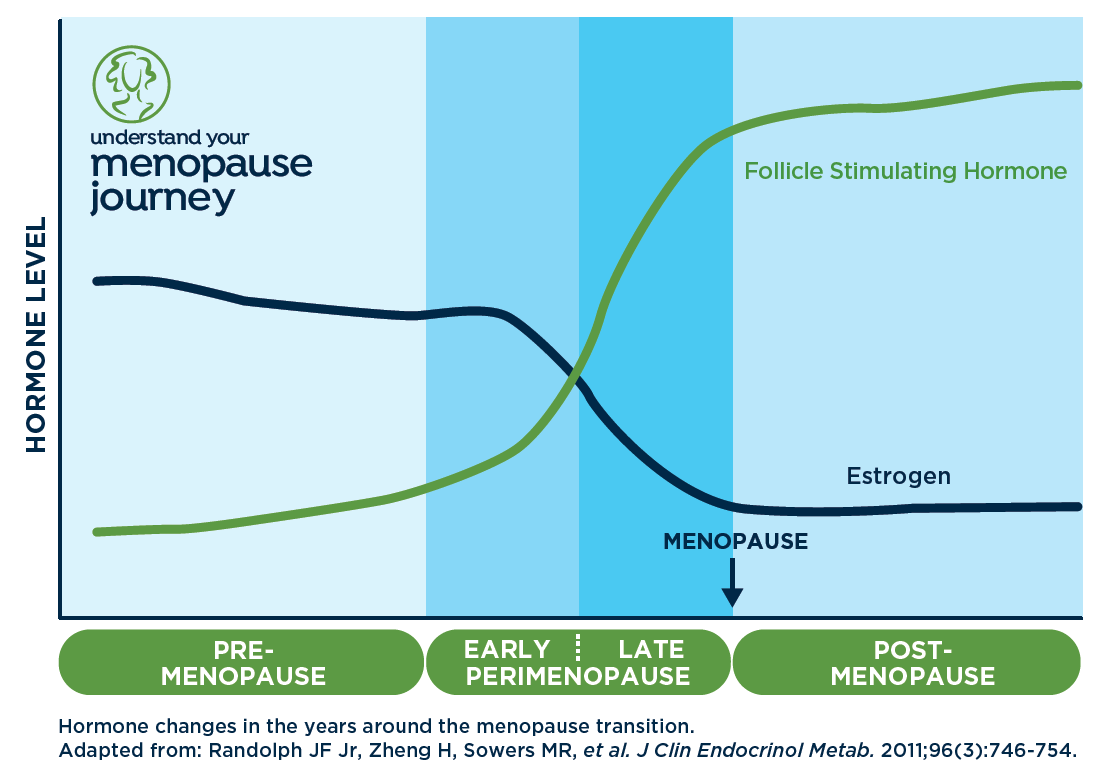
Hormonal Shifts
The main driver behind menopausal changes is the decline in hormone production, primarily estrogen. Estrogen plays a huge role in maintaining the health and elasticity of tissues throughout your body, including your labia and vaginal area. As levels of this hormone decrease, so too do many of its supportive effects. It's almost like a key ingredient slowly being removed from a recipe.
A Natural Process
It’s important to remember that menopause is a completely natural biological process, not an illness. Every woman who lives long enough will experience it. The changes you notice are simply your body adjusting to a new hormonal balance. It's a bit like the seasons changing, really; a natural progression.
What Happens to Your Labia During Menopause?
Now, let's get to the heart of the matter: what happens to your labia during menopause. The shifts can be subtle for some, more noticeable for others, but they are a very common part of this life stage. Many women, you know, just don't talk about these things openly.
Changes in Appearance: Shrinkage and Thinning
One of the most frequently observed changes is a reduction in the size and fullness of both the labia majora and labia minora. They might appear thinner, flatter, or even shrink. This is a normal part of the process, and, honestly, nothing to be alarmed about. Your body is just adjusting.
Loss of Fat and Collagen
The labia majora, in particular, contain fatty tissue that gives them their plumpness. As estrogen levels fall, this fatty tissue can diminish. Similarly, collagen, a protein that provides structure and elasticity to skin, also decreases. This reduction in both fat and collagen contributes to the thinning and shrinking appearance. It’s like a balloon slowly losing its air, just a little.
Color Changes
You might also notice a change in the color of your labia. They can become paler due to reduced blood flow and thinning of the skin. This is, apparently, a common occurrence, reflecting the shifts happening within the tissues themselves. It's really just another sign of the body's adaptation.
Changes in Sensation and Comfort
Beyond appearance, the changes can also affect how your labia feel. Many women report increased dryness, itching, or general discomfort in the area. This can be quite bothersome, and, you know, it's something worth addressing.
Dryness and Itching
Estrogen helps keep the labial and vaginal tissues moist and lubricated. With less estrogen, the skin can become much drier, leading to itching, irritation, and a feeling of tightness. This dryness can be persistent and, frankly, quite annoying. It's a bit like having dry skin anywhere else on your body, but in a more sensitive spot.
Increased Sensitivity or Discomfort
For some, the thinning skin can become more sensitive to friction from clothing or daily activities. Others might experience a general feeling of rawness or tenderness. This heightened sensitivity can make even simple movements feel uncomfortable, so it's something to pay attention to. It's, in a way, your body telling you it needs a little extra care.
Pain During Intimacy
The dryness and thinning of the labia and vaginal tissues can make sexual activity uncomfortable or even painful. This condition is often referred to as genitourinary syndrome of menopause (GSM). It's a very real concern for many women, and, honestly, it can impact intimacy quite a bit. But there are, thankfully, ways to help.
Impact on Protection and Function
The labia's protective role can also be affected by these changes. When they become thinner and less full, their ability to shield the delicate inner structures might be somewhat reduced. This is, naturally, something to consider for your overall intimate health.
Reduced Natural Barrier
The labia typically form a protective barrier, helping to prevent bacteria and irritants from entering the urethra and vagina. As they thin, this barrier might become less effective, potentially leading to a slightly higher risk of certain issues. It's not a huge change, but it's something to be aware of, you know.
Urinary Symptoms
The tissues around the urethra also rely on estrogen. So, thinning in this area can sometimes contribute to urinary symptoms like increased frequency, urgency, or even recurrent urinary tract infections (UTIs). This is all part of the broader picture of genitourinary syndrome of menopause, and, in fact, it’s quite common.
Why Do These Changes Occur?
The primary reason for these labial changes is the decline in estrogen, but there are other factors that play a part. Understanding the "why" can often help in finding the "how" to manage these shifts. It's really about getting a full picture of what's going on inside your body, so to speak.
Estrogen's Role
Estrogen is crucial for maintaining the plumpness, elasticity, and moisture of the labia and vaginal tissues. It supports blood flow to the area, encourages collagen production, and helps keep the skin hydrated. When estrogen levels drop during menopause, these supportive functions diminish, leading to the changes described. It’s a pretty direct cause and effect, honestly.
Blood Flow and Tissue Health
Reduced estrogen can also lead to decreased blood flow to the vulvar and vaginal tissues. Good blood flow is essential for tissue health, delivering oxygen and nutrients. Less blood flow means the tissues might not regenerate as effectively, contributing to thinning and a loss of vitality. This is, actually, a significant factor in how the tissues change over time.
Managing Labial Changes: Practical Tips and Support
While labial changes are a normal part of menopause, you don't have to simply endure any discomfort. There are many strategies and treatments that can help manage symptoms and improve your comfort and quality of life. It’s all about finding what works best for you, because, you know, everyone is a little different.
Moisturizers and Lubricants
For dryness and irritation, over-the-counter vaginal moisturizers can be very helpful. These are designed for regular use to hydrate the tissues. Lubricants, on the other hand, are used during sexual activity to reduce friction and discomfort. Look for products that are free of harsh chemicals, fragrances, and glycerin, as these can sometimes cause further irritation. This is, quite simply, a first step for many.
Hormone Therapy Options
For more persistent or severe symptoms, medical treatments can offer significant relief. These often involve some form of hormone therapy. As "My text" indicates, "We seek the best possible medical care for ourselves and our families," and this applies to menopausal health too. It’s about finding the right support for your body.
Local Estrogen Therapy
Low-dose vaginal estrogen is a very effective treatment for labial and vaginal dryness, thinning, and discomfort. It comes in various forms, such as creams, rings, or tablets, inserted directly into the vagina. This type of therapy delivers estrogen right where it's needed, with minimal absorption into the bloodstream. It's, apparently, a very targeted approach.
Systemic Hormone Therapy
For women experiencing a broader range of menopausal symptoms, including hot flashes and night sweats, systemic hormone therapy (HT) might be considered. This involves taking estrogen (and often progesterone) orally or through a patch, affecting the whole body. It can also help with labial and vaginal changes, naturally. This is a bigger step, and something to discuss carefully with a healthcare provider.
Lifestyle Adjustments
Simple daily habits can also make a big difference in managing comfort and supporting overall intimate health. These are easy changes that, honestly, can have a surprisingly positive impact.
Gentle Hygiene
Avoid harsh soaps, douches, or scented products in the vulvar area, as these can strip natural oils and worsen dryness and irritation. Use plain water or a very mild, pH-balanced cleanser. It's about being kind to your delicate skin, you know.
Comfortable Clothing
Opt for breathable cotton underwear and loose-fitting clothing to reduce friction and allow air circulation. Tight synthetic fabrics can trap moisture and heat, potentially increasing irritation. This is, basically, about giving your body some room to breathe.
Staying Hydrated
Drinking plenty of water supports overall body hydration, which can indirectly help with tissue moisture. It's a simple step, but, in fact, it's a good one for your whole body. Your skin, including the labia, will thank you.
Pelvic Floor Physical Therapy
A pelvic floor physical therapist can offer personalized exercises and techniques to improve blood flow, muscle tone, and flexibility in the pelvic area. This can be particularly helpful for discomfort related to tightness or pain during intimacy. It's a specialized approach that, surprisingly, can offer a lot of relief.
When to Talk to a Doctor
If you're experiencing persistent discomfort, pain, bleeding, unusual discharge, or if these changes are affecting your quality of life, it's a good idea to speak with a healthcare provider. They can rule out other conditions and discuss the most suitable treatment options for you. They are, essentially, there to help you figure things out. Don't hesitate to reach out for support, because, honestly, you deserve to feel comfortable.
Dispelling Common Concerns and Embracing Change
It's natural to have questions and even some worries about changes to your body. However, many of these concerns can be eased by understanding and acceptance. This is, you
What happens during menopause? - Clearblue®

What Happens To Your Body During Menopause
.png?ixlib=gatsbyFP&auto=compress%2Cformat&fit=max&w=1080&h=1080)
What Happens To Your Vagina During Menopause?